“Sometimes the most important thing in a whole day is the rest we take between two deep breaths” – Etty Hillesum
While the cases of COVID-19 are surging everyday, the only way the situation is being handled in the current scenario is by pushing lakhs of healthcare workers in the system. Health care workers are not only tirelessly treating a flood of critically ill patients during a pandemic but are risking their own as well as the lives of their loved ones, witnessing higher rates of death and experiencing breakdowns of protocol and support. The healthcare workers on COVID-19 duty are experiencing exhaustion and burnout (Nandan & S, June 2020).
As published in a British medical journal, with continuous and prolonged exposure to excessively demanding situations and feelings of uncertainty can lead to burnout, characterized by diminished vigilance, and increased safety lapses place clinicians and patients at higher risk for errors (Imo, 2017). While it is difficult to spot the symptoms of burnout, it is important to address even the slightest sign of stress often expressed as anger, irritability, restlessness, feeling overwhelmed, irregular sleep, racing, or constant worry.
This article is an attempt to elaborate on the concerns and issues faced by the frontline workers and a brief guidance on identifying stress responses and navigating through the phase towards better self- efficacy.
Words coming from doctors and surveys:
A veteran doctor reaching out to SWAASTHI mentioned about the overwhelming experience of treating incredibly sick people in stressful conditions of being into the PPE kit for 8 to 10 hours and piles of documentation that is leaving them with no time to think or feel anything. He also stressed on the importance of connecting with their family and friends at the end of the day to be their only ray of relief.
“There is always a constant fear that runs in my mind that what if I am spreading the deadly coronavirus to my children, who diligently follow the hygiene guidelines as suggested by the health bodies”, said Dr. Sachin Bajaj, Internal Medicines, Ujala Cygnus Orthocare Hospital, New Delhi ( as cited in “Doctor’s Day: How coronavirus”, July 2020).
The COVID-19 has been posing as a unique long-term stressor and risk for clinician’s physical, mental, spiritual and emotional well-being. Jessica Gold, a psychiatrist at the Washington University School of Medicine at St. Louise and many other experts express the possibilities of health care workers developing high rates of anxiety, depression, substance use issues, acute stress and, eventually post-traumatic stress as a result of what they are experiencing on the pandemic frontline. (Jillian, 2020).
“For doctors, mental health endurance is far more important than physical endurance. Healthcare workers have not seen their families for a long time and feel like their work is not appreciated”, said the COVID-19 nodal officer for Haryana and head of pulmonary and critical care medicine at PGIMS Rohtak ( as cited in Nandan & S, June 2020)
Stress Continuum Model – Know Your Zone:
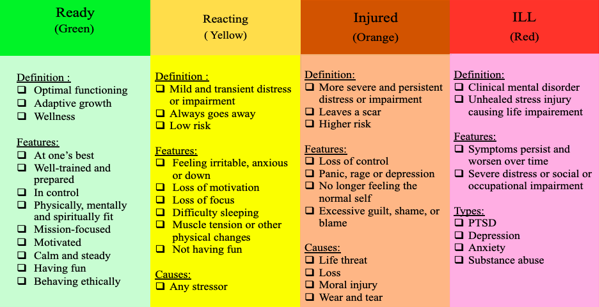
Fig1: Stress Continuum Model (Source: Naval Centre for Combat and Operational Stress Control, as cited in “The Stress Continuum”, 2019)
Feeling of burnout initiates gradually with triggering events stacking up the feelings of stress and anxiety. A good understanding of its aetiology and the process of development facilitates its early recognition, prevention and treatment. A quick look on the Stress Continuum model explains the movement from Mild to Chronic stress.The development of the stress continuum model lies with the Navy and Marine Corporation’s efforts to promote psychological health in the situation of crisis and stressful situations. While the Green zone doesn’t indicate absence of stress, it shows that the person is mastering stress through effective coping skills. The Yellow zone shows some reactions to normal stressors of life. Movement towards the Orange zone is alarming as it indicates stress injuries- damaging mind, body or spirit. The red zone is a clear indicator of the presence of stress illness and should be diagnosed by professionals. It indicates the need for help (Wise et al., 2012).
There is research based evidence reflecting the impact of pandemic on the stress level of the health care workers. A survey of 1,257 physicians and nurses during the peak of COVID-19 pandemic in China found that about 50 percent of respondents reported symptoms of stress, 44 percent reported symptoms of anxiety and 34 percent reported insomnia (Mock, 2020).
Similar situations are surfacing in India as well. “A large proportion of healthcare professionals, especially doctors, are experiencing symptoms of anxiety, depression, insomnia, and psychological distress. They report severe symptoms, which should not come as a surprise, as they often must engage in a lot of emotional labour, like reassuring patients, while keeping their own emotions in check,” said Dr. Shweta Sharma, Consultant-Clinical Psychologist, Columbia Asia Hospital, Gurugram (as cited in “Doctor’s Day: How coronavirus”, July 2020)
Despite such high rates of concerns experienced by the health care workers, they are typically unlikely to seek help. Among the several issues preventing from reaching out for help the significant ones are lack of time during this period, stigma attached to psychological issues and fear of losing faith and trust on themselves as health care providers
How to prevent burnout:
Many studies show that the right support at the preventive stage not only helps with the slowdown of movement towards the red column on the stress continuum, but it can also foster resilience. As Morganstein (as cited in Mock, June 2020) has mentioned, “Some people will find they experience a sense of an increase in their own confidence or ability to manage future stress.”.
Though stress in the current situation is unavoidable, it can be trapped at an initial stage by some simple but effective practices:
- Know that what you’re feeling is a normal stress response: Health care professionals are encountering continuous stress in the form of handling critical patients, loss of patients to death, practicing triage, working long hours and extended separation from the loved ones. As a result health care workers are experiencing an increased frequency of stress response. Practice self-compassion and give yourself grace, as all the medical professionals working during this time of crisis are experiencing distress (Shedrick, June 2020).
- Engage in consistent self-reflection to identify the mental and emotional signs of stress: Take a few moments at different points throughout the day for a personal mental health check-in. It may feel as if there is no time to spare, but this is a critical measure to manage stress (Shedrick, June 2020).
- Take a break and do things to uplift your mood: Watching short video clips with the essence of comedy plays a significant role in altering the state of mind from negative to positive. A good laugh is followed by a better mood (Shedrick, June 2020).
- Incorporate sensory-soothing techniques to facilitate calm and relaxation: Research supports the effectiveness of embracing sensory-soothing activities to calm the nervous system and promote healing from trauma. Be intentional in taking out time to practice some sensory-soothing activities like listening to your favourite music, visualising places where you feel at peace, and imagine your favourite culinary aromas that trigger meaningful memories (Shedrick, June 2020).
- Exercise: a simple stretch, mini exercise or short walks are effective and convenient ways to lift up the mood (Santi, 2020).
- Eat a balanced meal: Sounds difficult in the current situation but an addition of salads and fruits may contribute a significant addition towards a balanced meal (Fraga, 2019).
- Practice good sleep: Our body needs time to set and reset. According to the National Sleep Foundation, giving a small time for meditation or deep breathing relaxes the brain and body and promotes sleep hygiene (as cited in Fraga, 2019).
- Ask for help: During stressful times it’s important to reach out for help. It’s often difficult to reach out for help due to stigma attached, but at any point of time connecting with friends and family or sharing concerns with colleagues can help significantly. Teletherapy, helplines, meditation apps and other virtual health services have already made inroads and they are serving as common tools for reaching health care workers as well (as cited in Fraga, 2019).
How SWAASTHI can help:
iCALL is a helpline with trained counsellors and psychologists who are ready to serve the population experiencing mental health concerns. Understanding the current conditions and circumstances under which health care providers are working, iCALL in collaboration with UNFPA, has started a dedicated helpline for frontline warriors with the name of SWAASTHI, where they can talk to trained counsellors and psychologists without the fear of confidentiality being breached and seek support for mental and emotional concerns and referral linkages needed during the time of crisis.
Services at the helpline are available between 10am to 6pm from Monday to Saturday on the number 9152987824. It is a free service with no added charges for the session. The telephonic counseling is available in different languages like Hindi, English, Marathi, Bengali, Malayalam, and Kannada.
Allowing ourselves to seek help in our moment of distress is one of the most courageous steps we can initiate to aid ourselves with more resources.
References:
Doctor’s Day: How coronavirus has made life an emergency drill for medics. (2020, July 1). Business Standard. Retrieved from https://www.business-standard.com/article/health/doctor-s-day-2020-in-india-how-coronavirus-has-made-life-an-emergency-drill-for-corona-warriors-120070100210_1.html
Fraga, J. (2019, April 24). A Guide to Burnout. Healthline. Retrieved from https://www.healthline.com/health/tips-for-identifying-and-preventing-burnout
Imo, U. O. (2017). Burnout and psychiatric morbidity among doctors in the UK: A systematic literature review of prevalence and associated factors. BJPsych Bulletin, 41(4), 197–204. DOI: https://doi.org/10.1192/pb.bp.116.054247
Mock, J. (2020, June 1). Psychological Trauma Is the Next Crisis for Coronavirus Health Workers: Hero worship alone doesn’t protect frontline clinicians from distress. Scientific American. Retrieved from https://www.scientificamerican.com/article/psychological-trauma-is-the-next-crisis-for-coronavirus-health-workers1/?error=cookies_not_supported&code=0d5322ec-87bd-416b-b6a4-1fe401b1cd44
Nandan, R. & S. S. (2020, June 14). Doctors in covid-19 wards at risk of burnout. Livemint. Retrieved from https://www.livemint.com/news/india/after-three-months-doctors-in-covid-19-wards-complain-of-burnout-11592132659132.html
Santi, J. (2020, June 23). Emotional Burnout Is Real: Here’s How to Heal. The Everygirl. Retrieved from https://theeverygirl.com/emotional-burnout/
Shedrick, E. D. (2020, June 5). 7 tips for managing stress, burnout during the COVID-19 crisis. Clinical Oncology News. https://www.clinicaloncology.com/COVID-19/Article/06-20/7-Tips-for-Managing-Stress-Burnout-During-the-COVID-19-Crisis/58390
The Stress Continuum. (2019, May 20). BrainLine. Retrieved from https://www.brainline.org/article/stress-continuum
Wise, E. H., Hersh, M. A., & Gibson, C. M. (2012). Ethics, self-care and well-being for psychologists: Reenvisioning the stress-distress continuum. Professional Psychology: Research and Practice, 43(5), 487–494. DOI: https://doi.org/10.1037/a0029446











